There are few things in the world more frustrating than talking to average people about healthcare, but surely one of them is talking to fellow libertarians about the problems with our healthcare system. This goes beyond frustration with the typical libertarian infighting. Part of it is that there are so many things terribly wrong with our healthcare system, any libertarian can point to most any aspect of the system and find some legitimate confirmation that their favorite peeve is, in fact, a problem. However, even though there are numerous contributing factors to our healthcare woes, there is one evil to rule them all—but very few libertarians seem to understand what that is. The purpose of this analysis is to identify the ultimate cause of our problems, show why most libertarians’ favorite solution doesn’t really address it, and show why the Ryan plan is a hell of a lot better than most libertarians seem to appreciate.
What the Chart Does and Doesn’t Say
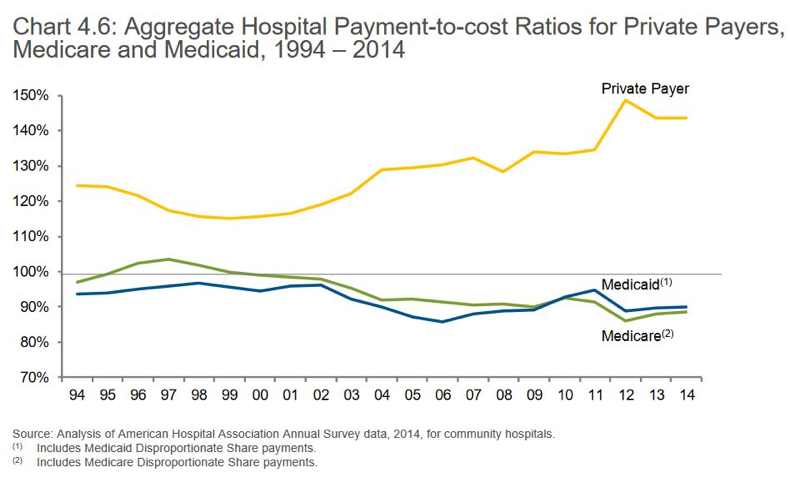
So, here is the ultimate source of the problem—Medicare and Medicaid only pay for a fraction of the cost of care. Providers are left to gouge private insurers and out of pocket patients for all the money they lose treating Medicare and Medicaid patients. According to the chart, hospitals are charging private pay patients about 150% of cost.
There are two major implications of this that people don’t generally appreciate. More charts would probably only make things more confusing, just understand two things: 1) Medicare and Medicaid patients are more expensive than private pay patients, and 2) the unfunded costs of Medicaid aren’t evenly distributed across the country.
What the hell does that mean?
- Medicare and Medicaid patients tend to cost more than private pay patients. People on Medicare are older and need more in the way of expensive treatments—heart surgeries, terminal illnesses, etc. Poor people on Medicaid, likewise, tend to have more babies, more health problems, and may generally be more expensive to treat than private pay patients.
So, don’t be confused by the averages in the chart—Medicare and Medicaid are covering 85% of the costs (on average), but they’re also covering more expensive costs. In other words, if the average private pay patient goes to the hospital once a year for an MRI scan, when the insurer pays 150% of that relatively small cost, they’re reimbursing that provider for the tens of thousands of dollars the provider lost performing heart surgery on someone with Medicaid or Medicare.
- The unfunded costs of Medicaid are not evenly distributed, and that points to another problem caused by Medicare and Medicaid only reimbursing providers for a fraction of the cost of care. Medicaid is for poor people, and poor people aren’t evenly distributed in your city, much less your state.
Hospitals are like retailers in that they serve a local community and that community has a particular income level. If the hospital is in an area with a disproportionate percentage of poor people, then there are few private pay patients in that community on insurance to make up for the shortfall. That means where the chart says that the average private pay patient is paying 150% of cost vs. Medicare/Medicaid’s 85%, it assumes that the patient mix is the national average.
In other words, if the hospital is an area where the local population only has 10% private pay patients and 90% Medicare and Medicaid patients, then that 150% percent of cost figure for private pay patients is going to be much, much higher–and those kinds of patient mix numbers are not uncommon in urban poor areas.
Sensitivity Analysis
The part where you all get mad at me!
Usually, a sensitivity analysis would show how taking the Medicare and Medicaid reimbursement rate up higher would impact the local cost of care. This sensitivity analysis is more about how the system would improve relative to various solutions. How would doing x, y, or z improve the situation?
For instance, wouldn’t the system be better if individuals and insurers formed the market instead of getting insurance through employers? I suppose it would be better, but that solution doesn’t address the real cause of the problem. Insurers would still be competing to sell you a policy that covers 150% of the cost of care (national average).
What about removing the “Cadillac” tax, getting the AMA to stop limiting class sizes of nurses and doctors, making pricing transparent, or making policies portable across state lines? Without getting into too much detail, transparency and portability are extremely complicated because of Medicaid, and even if those things were possible—what would any of them do about the fact that insurers are still paying 150% of cost (national average)?
Solutions
I suppose a lucid progressive might suggest taxing productive workers to take Medicaid’s and Medicare’s reimbursement rate up to 100%, but 1) raising people’s taxes so they can afford to buy insurance is just playing an especially stupid shell game with costs, 2) Medicare and Medicaid spending already make up almost a third of the federal budget, 3) the Medicare rolls are already set to increase as baby boomers continue to retire, and 4) that might be an extra $300 billion a year in real payouts—something like the size of our national interest payment.
The ultimate solution is to cut these programs.
Medicare is more politically sensitive, and Medicaid is especially responsible for driving up the cost of private insurance in economically distressed areas. Certainly, rolling back the ObamaCare Medicaid expansion is a necessary step before we can cut back the rest of Medicaid—and did you know there is a plan being considered in Congress, right now, that gets rid of the ACA Medicaid expansion after 2019?
Whatever else the Ryan plan isn’t, it’s one of those rare situations in which the actual cause of the problem is actually being addressed.
You still haven’t address why I’m wrong.
Other than my horrible Englishing skills
I muchly have wrong Englishing, m’self aye!
But your Scottish is perfect.
It is no enough good.
Yes, but as a bureaucrat, it’s almost a given that even if you know the right answer, you are still going to do the opposite.
713 East Wrongview Lane, Wrongityville, NW 00000
123 Fake Street, home of knifey wifey!
Wait, wrong address.
Can you provide a link to that address?
*runs away quickly*
*narrows gaze*
…
Awards “Bronze Shit-Stirrer” Medal.
Wrong!
You’re Wrong
You’re always wrong. There’s no why about it. :-p
This is an interesting analysis, and your point is well taken. I’m not mad at you, I just think you’re not necessarily addressing the argument you’re anticipating.
You mention that Ryan’s plan rolls back the Medicaid expansion. Did you know that there’s another plan, an alternative plan, that not only rolls back said expansion but also enacts the policy reforms you mention earlier in the piece that would improve outcomes and reduce costs if, as you accurately point out, they occur in conjunction with Medicare/Medicaid reform?
Medicare/Medicaid are a big part of the problem with healthcare costs in this country, but they’re not the only problem, nor are they the root cause, and I think this is where you err in your argument. Reform on those fronts are absolutely necessary, but that’s not in and of itself a complete solution. There is an inflationary effect on medical costs that is generated by a number of factors addressed in the Paul plan that are left untouched by the Ryan plan.
I’m sure I prefer the Paul plan, but the Paul plan hasn’t cleared committee and isn’t being voted on today.
I hope the Paul plan gets amalgamated into the final version through the joint/reconciliation committee.
There are two main features I want in the bill.
1) No more individual mandate.
I oppose the individual mandate on moral grounds. I’d oppose any ACA revision bill that didn’t address the individual mandate.
2) I’d support getting rid of the mandate even if it didn’t roll back the ACA Medicaid expansion–but the problems with our healthcare system aren’t really being addressed if they aren’t rolling back the Medicaid expansion.
There are plenty of other things I hate about the ACA, but if addressing those right now is too controversial to get passed, we can keep fighting for those revisions even if we don’t get them right now.
ObamaCare properly understood was a means to force especially younger healthier Americans to but insurance they don’t need and won’t use in order to let Obama expand Medicaid without breaking the insurance companies. Undong the Medicaid expansion is repealing ObamaCare, but no one in a swing state wants to go on the record and say that. If Ryan is moving that mountain on the sly, then I’m impressed.
. . . even if he isn’t getting rid of the Cadillac tax, etc. right away and right now.
Medicare and Medicaid, along with the HMO requirements that came out of the Clinton era all add huge bureaucratic requirements to medical billing procedures.
That is a major driver in medical costs as well.
Ken, one other thing I might question… As to your graph, the 100% baseline that you used is arbitrary and subject to gaming by the many actors in this comedy of errors. I’m sure the proportioning is right, but medical care is THE growth industry in the US. If the industry were losing 15% on 90% of their business, that wouldn’t be true.
I’m not sure what you mean by saying that medical care is the growth industry. Are you talking in terms of employment? Certainly, Medicaid and Medicare do a better job of reimbursing doctors for office visits than they do reimbursing hospitals.
In terms of the industry losing 15% on 90% of their business, I didn’t intend to suggest those numbers were typical industry wide. I’m saying that those numbers aren’t especially uncommon in areas of great poverty, where they can’t find enough patients in their local community to make up for the shortfall in Medicare and Medicaid patients.
Here’s an interesting article that, although steeped in progressive thinking and rhetoric, can’t really ignore reality.
“Since 2003, 16 hospitals have closed around New York City, four in Brooklyn alone, putting more and more pressure on the remaining hospitals to see more patients under more crowded and facility-challenged conditions. For families living in poor neighborhoods, more hospital closings have put greater pressure on the surviving facilities, and they have also stretched the distances people have to travel to receive care.
. . . .
For Judy Wessler, a long-time health care advocate, the hospital closings and consolidations were compounded by the state cuts to Medicaid reimbursement in 2012, exacerbating the financial fragility of the safety-net hospitals and putting care, and jobs, in jeopardy, something, she says, the state has not taken fully into account.
. . . .
As a way to remediate the problem, the state has been doling out dollars to those hospitals, but it’s been ineffective, Wessler insists. Instead of fully funding Medicaid reimbursement, the state is providing dollars “to keep the institutions open, but limping along,” says Wessler.
On the last day of December 2016, Gov. Andrew Cuomo vetoed a bill that would have increased the reimbursements to hospitals that provide a disproportionate share of care to Medicaid patients as well as uninsured patients. The bill, despite being supported by both legislative houses in Albany, would result in “increased and unbudgeted costs to the Medicaid program”
http://citylimits.org/2017/01/04/hospital-closures-and-medicaid-shifts-took-toll-on-nycs-health/
Growth industry?
More people are seeking care with subsidies and the individual mandate–if that’s what you mean?
I’d like to know how “costs” are determined. For example, I recently completed 50 hyperbaric treatments. The hospital billed my insurance close to $200,000.00 and my insurance paid the “agreed” cost of roughly $78,000. So if my insurance paid 150% of “cost” then the cost was around $52,000? I imagine that hyperbaric chambers aren’t cheap but there were four in a room, always occupied, and as soon as one patient came out they had another patient ready to pop right in. They kept those things loaded from 6:30 a. m. until 5:00 p.m. Monday thru Saturday. The doctor billed separately, $320 per treatment although I only saw the doctor one day a week for maybe five minutes per week (I had treatments six days a week).
Billing is not cost. It’s important to understand that. Billing is almost like the sticker price on a car or the manufacturer’s suggested retail price. They use that number for reference purposes, but various payers only pay a percentage of that–unless you’re paying out of pocket.
Aetna tends to be one of the highest paying insurers; their average coverage used to be north of 80%. That meant that they had a contract price, and they would cover 80% of the contract price. The chart on this story is saying that paying this 80% of the contract price (between the hospital and Aetna) might average, nationally, north of 150% of costs.
Medicaid may pay an average of 12.5% of that billing amount. Medicare may pay 25%. That isn’t 25% of cost. That’s just 25% of the “sticker price”.
The rates for insurers are often tied to the rates set by bureaucrats in Washington DC–it’s just that the insurers pay 70% or 80% of that “sticker price”. I am rusty as hell (no longer in the industry), but as I recall, it used to come from CMS:
https://en.wikipedia.org/wiki/Centers_for_Medicare_and_Medicaid_Services
Those guys use various criteria for setting rates, some of which are politically sensitive. They may pay more for prenatal care than they do for something that doesn’t involve pregnancy, mothers, and babies. AIDS treatment gets a ton of money.
Every quarter, outpatient procedures are updated with rate changes, inpatient stays per diem are updated, how many days you can stay in the hospital for each diagnosis, even the flat file for which codes can’t be billed together are updated quarterly. There is an entire profession, called a “coder”, someone who goes over each patient chart and matches it with these thousands of diagnostic codes, tying that patient stay to a reimbursement rate. I used to help make the software that would help them do that. It’s incredibly complicated. If the servers they run it on weren’t calculating patient billing, they’d be doing weather forecasting, nuclear testing, traffic modeling, something heavy like that.
The insurance companies typically use the same codes and rates as Medicare and Medicaid–but they pay different percentages of those rates. This is further complicated by PPOs, for instance, who have contracts with various hospitals limiting maximum payments, which procedures will be done, etc.
How does CMS set the rates?
Like I said, some of it’s political. They tend to fund things that will get in the news well if they weren’t well covered. Apparently, they take their budget for the next year into consideration, look at the payment averages from all the hospitals across the country (all hospitals are required to file those), and then . . . they use whatever criteria central planners always use. Sometimes, their decisions don’t make any sense. Most rates don’t change for procedures every quarter. The changes are published in the Federal Register. Reading it and understanding what the changes mean can be a real challenge by itself.
You can’t look at your bill and have any idea how much it really cost. Not even a coder could do that. They can tell you what the reimbursement rates are, but they have no idea about the real cost. That comes from accounting rather than billing. They’re even under different departments. The CFO may not be able to tell you anything about how billing works, and the Health Information Management Department is clinical. The Medical Records Director typically answered to the Director of Nursing–not the CFO.
Look how much money they make:
http://www1.salary.com/Medical-Records-Director-salary.html
That’s a four year degree.
Sorry for the late reply, work actually started to happen.
I hear what your saying, and part of me agrees. Something is better than nothing, and maybe we wind up with some happy medium between the Ryan and Paul plans that can form the basis of further reform later down the line. But part of me is also afraid that there’s one and only one shot at this, and if Congress blows this opportunity now, it’s never going to come back. I mean, I can just hear the progs now: “You want to pass *another* healthcare reform bill? You didn’t get it right the first time?”
And then also I just don’t see the Ryan plan as substantially addressing the problems that Obamacare was arguably meant to address or the problems it created in passage. There are two components to health care being crappy: cost of healthcare itself, and cost of insurance. Ocare addressed the latter in the short-term for a few people by aggravating it for most other people, and it pretty much just ignored the former. The Ryan plan undoes some of the damage to the latter, and still does nothing about the former. The Paul plan is the only proposal that addresses both.
But like you said, maybe a miracle happens and the plans merge in some fashion.
The worst thing ObamaCare did to the cost of care was to expand Medicaid.
What I’m trying to tell you is that the ultimate source of our problems is Medicare and especially Medicaid. The biggest reason that premiums continued to rise and deductibles went up after ObamaCare was because of the Medicaid expansion.
The more people there are on the Medicaid rolls, the more insurers get gouged to make up for the bigger shortfall. You see that uptick in the private pay line on the chart right after ObamaCare was passed? That’s about more people piling into Medicaid. Getting those people back off of Medicaid is a necessary step towards fixing the problem.
There is no solution that addresses the real cause of the problem that doesn’t include undoing the ACA Medicaid expansion, and the Ryan plan gets those people back off of Medicaid.
Oh, in addition, the Ryan plan gets rid of the individual mandate.
If the Ryan plan passes, we should all celebrate . . . and then get pissed off all over again and demand they do even more.
Before I read the post, I want to make it clear that I am not wrong.
Ken is wrong for having withheld this information from me for so long.
I talk about it all the time!
FWIW, I don’t claim expertise, here, but I do claim familiarity.
I worked reimbursement in a ghetto LA hospital for years–that had to close because we couldn’t attract enough private pay patients. It’s a nuthouse now.
I was also the quality control analyst for all the payer and grouper software for a company that does that software for some of the biggest hospitals and hospital chains in the country. I put together the reimbursement and reporting software–along with quarterly updates–all day every day for a long time.
That Medicare and Medicaid pay only a fraction of the cost of care is maybe the least known fact that affects the most people. There isn’t any aspect of our healthcare system that isn’t horribly distorted by that fact.
No one is wrong here, JB. Only misinformed.
Well, I’m usually wrong. Wrong, misinformed, stupid, fat, drunk……
Fat, Drunk and Stupid is no way to go through life.
That’s no way to go through life, son.
You can say that again!
Sounds like Hyperbole has a vested interest in Obamacare.
He has a side job as an Obamacare Navigator?
No, he needs the guaranteed issue (Fat, drunk,…)
This is likely a stupid question, but why are hospitals taking patients on whom they lose money? And why are insurers not raising a stink over being bilked by hospitals? Why IOW is such a backward, unsustainable payment model so baked in?
Because there’s a law forbidding hospitals from turning away patients. So these people would just turn up in the ER anyway, and some money is better than no money.
As for the insurance companies, if they can make the premiums add up to cover the outlay, they can stay afloat. I don’t think this disparity was there from the start, much like a tumor, it grew into the system.
I figured it for something like that. But it seems like insurers would be lobbying harder on this premise. Maybe they are and I have no idea, which wouldn’t surprise me.
Why do you think they lobbied for the individual mandate?
Also, most hospitals are non-profit organizations with stated missions that are things other than making money. They have to make money somewhere in order to lose money somewhere else, but the losing money on certain patients part is not necessarily a bad thing.
The insurance companies almost all lose money on insurance. Their profits are made on investments. I worked for Nationwide for years and we never had an ratio less than 100 on homeowners business. I can’t imagine what medical ratios look like for some of these companies.
Short answer: in many cases they are turning those patients away, and have been for some time. Doctors refusing to accept Medicaid patients has been an issue for decades, and with the ACA’s passage, many docs have stopped taking new Medicare patients as well.
Every hospital must maintain certification joint commission certification… https://www.jointcommission.org/faqs_ccn/
One of my mentors was director of nursing at Hopkins. Basically all the edicts that come down from high must meet the joint commission standards…there are dozens upon dozens upon dozens of full time paper pushers in every single hospital jumping through every loop to meet these standards for certification. There are “test” surveys and reports…you would not believe the amount of power jcho has. Since Medicare/Medicaid are the MAJORITY purchasers of services within any hospital they drive the market rates on the private sector as you stated.
Obamacare also flavored in “patient satisfaction” surveys to these edicts so now while my unit may have zero hospital infections if you rate quietness of the unit at night at 8/10, we fail according to “patient satisfaction”. Reimbursement will now be tied to quality of delivery (which I support to an extent…tho idiot patient populations who can’t follow instructions obviously not fair to compare to) but also if I didn’t give you an opiod to control your pain effectively; well I asked, but doc won’t prescribe because the DEA says he’s a drug pusher for writing too much pain pills for old ladies with new hips….here’s some Tylenol.
ZARDOZ SPEAKS TO YOU, HIS CHOSEN ONES. ZARDOZ IS PLEASED THAT BRUTALS NUMBERS MAY BE THINNED OUT BY GOVERNMENT INTERFERENCE IN MEDICAL FIELD.
Maybe I am being too simple-minded, but it seems to me we are never going to solve this when a large number of people think it’s cruel NOT to rob everyone else to pay for some poor saps heart surgery.
Ken mentions the supply/demand problem with doctors and nurses in the US and a few other areas where he believes there is only marginal gains via reform. My opinion is this: If we can’t get marginal reforms, we are truly fucked.
I was talking about this the other day, wondering why they can’t approach healthcare reform piece by piece, and fix the mess over a period of time with many smaller steps.
the short answer is, “because politics”. Its just another reason why govt regulatory controls turn into a neverending cycle of creating their own problems to fix. Because the process of “fixes” become so visible and high-stakes, no one is willing to risk spending years on tweaks, exposing themselves to risk and endless compromises, and instead tries to team up and solve everything in one big omnibus clusterfuck which guarantees that everything in it is being done purely for the optics.
It’s the same reason no government has ever successfully recovered from late-term bureaucracy.
I see you stopped smoking. Good timing, since Obocare guaranteed issue might go away.
That’s my “I’ve got 5 nicotine patches on my inner thigh” face
Amateur! You place the patches next to your throat. Mainlining the carotid gets it to your brain direct.
New Zealand was in remission for a few years in the 1980s.
A lot of it is driven by Medicare and Medicaid considerations.
Portability is complicated because various states implement Medicaid in various ways, and hospitals set up their individual programs so that they can maximize their funding under those reimbursement rules. Let people pay North County San Diego rates for insurance that’s good at New York hospitals, and those hospitals are in deep trouble. Meanwhile, if New York State didn’t have their own Medicaid system, those hospitals in poorer parts of the city and state couldn’t stay open–and there have been a large number of hospitals that have closed over the years for that reason.
Point is, many of the reforms people want can’t be implemented because of Medicaid and Medicare. You can’t charge everyone the same rate when providers can’t charge at cost for the majority of their patients. And the larger you make the Medicaid rolls, the worse it gets. It’s like once you decide to make Medicare and Medicaid such a big part of the system, all your other decisions are made for you.
The Soviet system was like that, too. There are undesirable consequences of running a system like that, and once you decide to run it like that, you don’t have much choice but to do x, y, and z. It’s like the head of Venezuela imprisoning bakers for not selling bread below cost. That sounds so crazy, but unless you’re going to reform the system, that’s what you’re going to end up having to do whether you want to or not.
True Story
Last week I had blood drawn for some lab work. When I went to pay I informed the kind lady at the counter that I was Self Employed and had no insurance because Obamacare and since I was paying cash if there were any price breaks for cash that I would certainly appreciate it. She smiled and said she heard that often. So she emailed the main office and a few minutes later got back a discount price for me. Insurance price $511.00, cash price $98.00. As I was paying I kept asking her questions and one of them was this. If I did have an Obamacare policy with it’s huge deductibles would I have had to pay the insurance price rather than the cash price ? She said that I would have had to pay the $511 full price because it represented a portion of my deductible. That makes sense to me but it is another of the many overlooked negative aspects of Ocare that gives people access to health insurance but not healthcare. Of course if I had been a non productive member of society it would have not cost me anything, deductible or premiums, to access healthcare.
A rational insurance policy would be for catastrophic coverage. Everything else out of pocket.
prior to Ocare I had BCBS with 2,500 deductible, 3k total out of pocket and 100% coverage after that. They paid 12k for shoulder surgery 5 months after I signed up. I could go to just about any doctor I wanted with no need for referrals to a specialist. Obviously the Grubers of the world thought I had it too easy.
I am sure the $511 is the price they bill to insurance, that then is reduced due to the deal with the insurance company to $178 or something. Which is still more than the $98, but not as crazy as the original amount.
And isn’t the $511 an artifact of Medicare which insists that its rate be a small percentage of book?
Nah. Its been a very long time, if ever, that Medicare paid based on discounted charges. Not many commercial contracts do that any more, either. Most commercial contracts are a percentage of Medicare (usually over 100%) these days. The prices in a hospital “chargemaster” are mostly an historical artifact that gets pulled out whenever you have the rare uninsured patient who can actually afford to pay their bill.
I talked with my insurance Co the other day because they weren’t covering my wife’s OB visits, and the office thought they should be covering 70%. Turns out we were in a catch 22 because of the move. Couldn’t have gotten insurance in the new state because we weren’t yet residents, yet didn’t have coverage because we were out of network since we moved out of state. Since you’re required to have a 2 week lead up to buy or cancel, we only had 2 weeks where we were eligible to get compensation from insurance, had I been on the ball and gotten it changed to a company in the new state within 3 days of buying our house out here.
Now we get to have the “what’s your best deal” discussion with the OB office so we’re not out $700 on top of the $1400 in premiums for 2 months of worthless insurance.
That sucks.
Attempting to do this is a big part of how we got here.
See outside of Paul and a handful of the Freedom caucus guys in the house no one in Congress has even a shred of a free market bone in their bodies giving them no chance whatsoever to accurately identify the actual problems or identify solutions with a potential for success so what you would get is a series of ineffective bandaids applies to the wrong parts of the system creating ever larger sets of problems to be solved similar to the HMO mandates of the past.
Maybe I am being too simple-minded, but it seems to me we are never going to solve this when a large number of people think it’s cruel NOT to rob everyone else to pay for some poor saps heart surgery
See, most people view government as the same as society. And they’re part of society, and, well, it’s just plain mean to tell someone else that they should die because they can’t afford healthcare. It’s the equivalent of labeling yourself some sort of scrooge. It’s the reason why an asshole like Bernie Sanders is consistently called a nice man so often as if he was personally going to spend his money to provide healthcare to the poor. So we all have to pretend that we don’t know a dozen or so irresponsible asses who have lived awful lives and who never had a care in the world over their health until it was too late. These people are just the unfortunate and oppressed when spoken about in the aggregate.
Jimbo, I’m not against those smaller reforms. I’m just saying they won’t solve the problem.
Not if the problem we’re talking about is the affordability of healthcare.
If a community hospital in a poor area needs to charge private pay patients 200% of cost in order to break even, even if you bring down the salaries of doctors and nurses by opening up class sizes and easing licensing, that hospital will still need to charge private pay patients 200% of whatever costs.
It should be noted, too, that some 70% of the community hospitals in this country, last I checked, were non-profit. There’s reason for that. If you’re losing money on every Medicare and Medicaid patient, You can’t make it up in volume. Again, we must move patients off of the Medicaid rolls. All the other solutions are more or less subject to that solution.
The ship sailed when we decided that we would socialize the cost of people’s individuality.
If we don’t course-correct soon, you will see more efforts to control behavior to keep costs down. It won’t be pretty.
In the individual mandate’s place is a mandatory 30% surcharge, payable to insurance companies, for those who go without coverage for a prolonged period of time and then choose to purchase another plan. This surcharge is wholly insufficient to fulfill its purpose. Whereas the individual mandate punished people for not purchasing insurance, the surcharge punishes people who’ve decided they do want to buy it. It
So, can I assume the “Healthcare/insurance isn’t a legitimate function of government, therefore our bill completely removes all government from the system” bill isn’t a starter?
That depends on how you feel about soul crushing disappointment.
The very notion would be considered absurd. That’s how far gone we are.
I spent 7 hours driving back from Salt Lake yesterday. Listened to Limbaugh and Hannity in their entirety (…I know). One of them made the comment that the biggest obstacle, IMO, to bringing down costs, pre-existing conditions, won’t even be addressed in this version, or in Rand’s for that matter. Neither side will touch it with a 10 foot pole. It has become enshrined in the untouchable mountain of free shit provided by the welfare state.
It’s so bad that even suggesting doing the right thing is met with ridicule.
Fuck them all. A pox on both their houses. Let it burn.
Let them eat cake.
Two points:
1) There’s something to the suggestion that Medicare, specifically, isn’t like insurance.
If you live long enough, the chances of you getting a terminal illness that’s expensive to treat or being in an accident that’s expensive to treat are very high. I suppose if you are killed in the accident, shoot yourself in the head, or the first heart attack is fatal, then you won’t need healthcare–but otherwise, the actuary at the insurance company isn’t calculating the odds of you needing healthcare; she’s just figuring out when you’ll need it and how much it will cost. Who in their right mind would sell standard health insurance to someone over the age of 70 based on the hope that you won’t need any care?
That’s the rationale for Medicare–no market can function.
I think there should still be a market for such care, but it would function more like the options market. The insurance company might trade healthcare like options with a strike price and an expiration date. Maybe you buy an option worth x amount of care with an expiration date, and every day it gets closer to the expiration date without hitting the strike price (you exercising it), just like with an option, there’s downward pressure on the value of the option in the secondary market. If you die before the expiration date, the option still has value on the secondary market. The further out the expiration date, the more the option costs to buy on the market.
Average consumers wouldn’t need to understand all that–it would be marketed to them like reverse mortgages or life insurance.
2) The market of ideas is like other markets in that you don’t dictate ideas to the market any more than competing manufacturers can dictate prices to a market. We can shift the Overton window through marketing, but we’ll always be limited by what the market will accept. Remember, market forces are people making choices. If we’ve got better product at lower cost than the competition, but the market is choosing someone else’s product, it isn’t that the market isn’t functioning properly. It’s a failure in our marketing efforts.
I think there should still be a market for such care, but it would function more like the options market. The insurance company might trade healthcare like options with a strike price and an expiration date.
Sounds a lot like term life insurance.
The pre-existing condition problem is a symptom of a larger problem: Employer-mandated health insurance which is stacked with guarantees, government subsidies and all-encompassing healthcare regulatory policy from the feds down to the municipality.
You COULD address the pre-existing condition before addressing the above causes, but it would be putting the cart before the horse, and you’ll never win because you’ll just end up looking mean.
I like this. Thank you.
Small quibble, but Medicaid reimbursement rates are determined by each state. What you’ve shown is an average of the Medicaid reimbursement rate, but in some states it is substantially lower than Medicare
Good article in general. Just wanted to point out that the situation is actually worse than you’ve laid out, in a few different ways:
1. In addition to covering the elderly, Medicare also covers care for a number of very expensive special populations. End-stage renal disease being one example.
2. In addition to covering the poor, Medicaid is one of the primary payers for end-of-life care, which is extremely costly.
3. Most ACA supporters were too busy fellating Obama to notice it, but one of the primary mechanisms by which the government expects to pay for the ACA is … wait for it … gutting Medicare. Unless that piece of crap is repealed, expect this to get a lot worse.
This. Once you spend all your assets but can’t care for yourself, you can get Medicaid to pay for your shit nursing home at 5-6k/day. Don’t worry, tho your brain is mush from dementia, we are still giving you those cholesterol and blood pressure meds….and the when you visit the regular hospital for community acquired pneumonia every 3 months, we treat that too at 10k or more a day (you need those super antibiotics to treat you drug resistant infection)…..
Imagine instead we said to a family when they got in Medicaid for their dementia family member…we will give you 20k if you agree to hospice now….
Maybe we will get there when all the states go broke as the boomers clog the rolls! This was before Medicaid expansion and muuuuch larger driver of its cost over the coming decades
http://urbanmilwaukee.com/2016/06/13/the-state-of-politics-medicaid-costs-are-unsustainable/
One state Medicaid for old ppl, but this problem is across all states
Oh, and Medicare and Medicaid (and my parents’ long-term care insurance) tried to dick Dad over when Mom went in the nursing home. Supposedly Medicare is supposed to pay for either 60 or 90 days while Medicaid makes a decision. Mom suffered a massive heart attack and died after eight weeks in the nursing home. (She was in the hospital one week while they were waiting for a nursing home spot to open up.) So right there everything should have been paid for. And if not that, the amount of LTC benefits they had paid for should have paid for it — the LTC plan would have paid about a third of the cost each year. But not long after Mom died dad got a ~$20k bill from the nursing home.
This illustrates what grinds my gears the most about health insurance (and like a few others here, I have a lot of first-hand experience of the industry through my work): insurance is great for basic preventive services and low-cost treatments, but when people experience a genuinely unforeseeable and expensive medical event, they often find they’re not as “insured” as they thought they were.
IOW, if you expect health insurance to work like insurance, you’re being scammed.
we will give you 20k if you agree to hospice now
+1 Death Panel
Seriously, though, no argument with anything you’ve written here.
While I agree Medicare/Medicaid costs are a serious issue, this is not the actual cause of our problem. The root cause of our healthcare expense is that we don’t have freedom of healthcare in this country. You are forced, under threat of imprisonment, to only seek medical care from members of a guild-like order. In turn, the numbers of members in this monopoly are kept artificially low driving up costs through the roof while reducing supply.
Imagine how cheap healthcare would be if you could see whoever you wanted and pay out of pocket for anything you wanted no questions asked. Worked well for the past 10,000 years of human civ in terms of cost and availability. There whole insurance question would disappear as you’d find new insurance plans pop up overnight that covered virtually every scenario imaginable.
Currently, the healthcare monopoly has allowed health insurance companies to work themselves as close as possible to the process until health insurance has effectively become indistinguishable from health care. Look no further than the mandate that costs for self-pay patients are not legally allowed to be less than the average rates charged for patients with insurance.
I appreciate that it’s practically impossible to escape health service or health supplies providers that don’t treat Medicaid or Medicare patients and, hence, don’t have any problems associated with underpayment. There are various reasons for that.
When the hospital I worked at was seriously in trouble, they started calling ambulances for people who turned up in the ER with only Medicaid–and send them to the community hospital ER on the other side of town. The local regulators threatened to close us down over that.
They wouldn’t let us operate without an ER either.
You cannot refuse service because of the inability to pay, and we couldn’t refuse service because the patients were on Medicaid either.
You’re right that there needs to be a private option, but as long as Medicaid continues to underpay, providers will be forced to compensate for that. The system you’re describing is, in reality, a system without Medicare or Medicaid. I’ve been to private hospitals that operate like that–in Mexico. It’s like checking into or out of a Hotel with a spa.
https://starmedica.com/home/es/index
No, that isn’t a hotel room, but staying overnight is less than a decent hotel in the U.S.
“Imagine how cheap healthcare would be if you could see whoever you wanted and pay out of pocket for anything you wanted no questions asked. Worked well for the past 10,000 years of human civ in terms of cost and availability.”
Nuh-uh! Healthcare was terrible before the government fixed it! I mean, we had the Black Death, Spanish flu, and polio!
/statist
So a quick review shows that Medicare/Medicaid account for 37% of total health spending. If the average reimbursement is 85% of cost, then Medicare and Medicaid are putting a 6% loss on the entire market before you even consider anything else.
There’s an old joke in manufacturing. We’re losing $20 bucks on every unit shipped, but we’re making it up in volume.
I was going to chastise you (or the editors or whoever you grabbed it off Google from) for making that chart a JPEG, then I saw that it was actually a PNG. You (or somebody) made it JPEG first and then converted the JPEG to PNG. The end result is the worst of both worlds, crappy image quality and bloated file size. That’s… impressive.
Just for you.
That came off whinier than I intended. To show I’m not trying to be a bad sport, here’s a better quality version.
It’s an omage to TSTSNBN’s renowned technical prowess. Why do you hate art kbolino?
Our usual image guy is in a diabetic coma and it went up in a rush with my shit computer skills. Deal with it tech boy.
I really need to work on not writing my comments like I would at TSTNBN.
My understanding (please correct me if I’m wrong) is that Ryan’s plan doesn’t get rid of the insurance requirements that are driving up costs (i.e forcing men to get maternity care coverage) and covers preexisting conditions, the second thing majorly driving up costs. Rand’s plan gets rid of the coverage requirements and compromises on preexisting conditions where it gives people a two year time frame to get coverage of their preexisting conditions. So, say someone loses their job and hence their insurance, they have up to two years to get insurance where the insurance companies have to cover the preexisting conditions. If the two years goes by, companies don’t have to cover them. This makes it so people don’t wait until they’re sick to get coverage. Ryan’s plan also doesn’t allow for insurance companies to compete across state lines as well.
The competition across state lines is a pipe dream in no small part because of Medicaid. For instance, some states help providers with their losses on Medicaid–like New York. If they didn’t, those urban hospitals would close, and the state wants them open so poor people have an ER and a hospital to go to. If someone is in Idaho or Vermont, their insurance company charges them based, in part, on the amount they expect to be gouged if you end up in the community hospital. When you’re in Vermont, where there are fewer people on Medicaid, they charge you one rate. If you end up moving to Philadelphia, and end up in a community hospital with a ton more of Medicaid patients, your insurance company is going to get so screwed . . .
It isn’t just from state to state that’s the problem, your insurance company is also afraid that you’re going to go to a hospital in your own state where they don’t have a contract that limits how much they can be charged. If you’re on Aetna’s PPO and you’re from the wealthy part of Los Angeles, they don’t want you going to King Drew Medical center on the other side of town–which is always going in and out of bankruptcy for lack of private pay patients. Opening up that problem nationally and across state lines would most likely drive the insurance companies to consolidate (less competition) and raise premiums dramatically to counter the unpredictability of how much they’re going to get reamed based on what state you land in.
Again, the real cause of that problem is Medicaid and, to a lesser extent, Medicare.
My understanding is that Ryan’s plan does get rid of the individual mandate. If you want to qualify for subsidies, then you need to maintain continuous coverage–to combat people jumping onto and back off of ObamaCare based on whether or not they’re sick at the time. That isn’t really an individual mandate any more than requiring people to buy insurance in order to qualify for coverage is an individual mandate.
The staff over at the other site are really confusing the situation.
Using the IRS to punish people for not buying insurance is not the same as requiring people to pay premiums in order to maintain coverage.
Is that problem handled by “in-network” “out-of-network”?
My out-of-network deductible and out-of-pocket are much higher than in-network. So I wouldn’t go to the cross town out-of-network hospital.
That’s exactly why they do that. People respond to price signals!
They often also want you to get pre-approved.
They typically have a clause in there that lets you off the hook if you’re admitted through the ER if you’re taken there after a car accident or by the paramedics after a heart attack. But if you have any choice in the matter, the premiums you pay were predicated on you limiting yourself to facilities with which they have a contract that limits their payments, the situations in which various treatments are covered, etc.
If you’re ever admitted through the ER into a hospital that’s out of network, watch out. They may give you every MRI, test, and procedure they can possibly justify–rather than just what’s needed. And even if your insurance company is still paying, say, an in network percentage of 80%, you’re still going to get a bill for the other 20% of the charges–regardless of whether you really needed those tests. And as the chart above shows, every dollar you end up paying of that bill is going to be some multiple of actual costs.
I’m late to the party here, but wondering… wouldn’t this Out-of-Network practice be a way to get around the issues of selling across state lines? If a plan were designed for the highly subsidized NY market, then anything out of NY becomes Out-of-Network and effectively costs more. Or would this not be as simple as I’m thinking…
I’m not mad Ken. Great, to the point article/blog!
Stimpy: (after the “Happy Happy Joy Joy” song) Ren. You’re… you’re angry?
Ren: You’re darn tootin’ I’m angry! I have never been this angry in my ENTIRE LIFE!!! (then he calms down) Hey! I feel great! I love being angry! Thank you, Stimpy.
Stimpy: (scared/confused) Happy to be of service?
(maniacal laughter from off screen)
It should be noted, too, that some 70% of the community hospitals in this country, last I checked, were non-profit. There’s reason for that. If you’re losing money on every Medicare and Medicaid patient, You can’t make it up in volume.
I hope you’re not using “nonprofit” and “operating at a loss” interchangeably, here.
Hehe… I remember getting into a knock-down dragout with a commenter at Reason about this. It’s amazing how many people believe they are one in the same.
I don’t think Ryancare was ever intended to pass. I think it’s a setup for 2018 election cycle. Randcare has more promise in my opinion.
Off topic but I do hope they fix the taxes for the better soon.
I don’t have a pithy way of phrasing this, but the idea of alienating key parts of your base with a controversial plan that you then can’t get passed despite controlling the entire federal government doesn’t seem like a sound strategy to me. It’s almost as bad as Ryan’s decision to go ahead with that photoshoot where he seemed to be going for the Samuel “Screech” Powers look.
Nobody claims Team Red or Blue are smart.
I once thought I was wrong, but it turns out I was mistaken.
Now I see the attraction to Snoopy.
Well, he is a flying ace.
Dammit!
-1 Sopwith Camel
That’s a John worthy typo. Also.
Nice article, Ken.
This just popped into my head. We all have heard about “OMG $100 for a fucking aspirin pill!”. How many people out there (aside from Bernie Sanders) seriously think room can be made through “price adjustments” to “fix” the high cost of health care?
An astonishingly large number unfortunately
*nods*
So, yesterday a chair from the House Intelligence committee discloses that yes, the previous administration was conducting surveillance of the Trump campaign…. and while the surveillance may have been ostensibly-legal, information-collected on non-targeted US-persons was being distributed ‘unmasked’ throughout government = very-illegal on the face of it.
And so i go to the WaPo and NYT, and – shocker – can’t find a single story anywhere (even tangentially) about the subject on the front pages.
the one i finally dug up (via searching) had this headline =
Nunes Puts Credibility of House Panel He Leads in Doubt
They loved Nunes when he said things that they could create headlines with to bash Trump. Hate him when he bolsters Trump’s claims. It’s a real shocker.
I thought I was at peak derp yesterday when the media was collectively freaking over the AP’s story on Manafort lobbying for a Russian oligarch in 2005 (who by the time of the Republican primaries, was claiming Manafort defrauded him and had cut all business dealings). They state that Manafort was doing the Kremlin’s bidding, or rather the bidding of pro-Putin factions in the Ukraine, in Washington despite not a single quote they provided actually directly stating anything of the sort. And this from the same media that told us Uranium One was a non-story despite, what, like $60 million going to the Clinton Foundation? Then they hit us with the Nunes spin and CNN’s piece of shit story.
The Dems and their whores in the media are just phishing here. They successfully got Sessions to get out of the way. Now they want the GOP Congress out of the way so they can get their special prosecutor.
You have to be a real simple minded fuck or a complete partisan hack to walk away from this coverage, especially the links provided, and not notice that much of the media are blatant mouthpieces for the Democrats.
One of the most remarkable rhetorical turnarounds by the media i’ve ever seen is the insistence that trump is “lying” when he mentions wiretapping…
…when that is the exact same nomenclature they used describing the exact same incidents of surveillance in January =
It’s like shooting fish in a barrel attacking them at this point. They are breathlessly implying some criminal wrong doing by Trump or his associates while blatantly ignoring the blatant crimes they document every time they report. The only actual criminal behavior seems to be from Obama holdovers. And the NYT’s itself outlined what sure as shit looked like a conspiracy to discredit the incoming administration with leaks.
I can’t believe that normal people give a fuck about any of this, though I do my best to avoid interacting with them so I’m stuck in the dark.
That is golden. Thanks for the link.
“I can’t imagine how Trump might have gotten the idea that his Aides were wiretapped. Maybe he READ THE FRONT PAGE OF THE NEW YORK EDITION OF THE NEW YORK TIMES?”
You cannot refuse service because of the inability to pay, and we couldn’t refuse service because the patients were on Medicaid either.
All the talk about ERs kind of bugs me, for this reason: if this “ER abuse” was really such a big deal, and a drag on operations, the hospitals would have devised a means of dealing with it. Not by dragging the dying out onto the sidewalk, but by improving their methodology for sorting and differentiating between actual emergencies, and “Mommy my tummy hurts” cases. Like an old-fashioned nurse at a desk in the doorway with a list of questions.
“You go through that door, you go through this door.”
Since there doesn’t seem to be such a solution, I can only assume the problem, or the incentive to fix it, isn’t as bad as some people would lead us to believe.
Maybe I’m all wet.
Isn’t that what triage is?
Depends on where you are, and what your general population does – in Chicago, people without the means will wander into a Cook County hospital and fill the ER. You won’t find that in a well off suburb.
Ultimately, you’re talking about turning people away who are in an emergency.
Sometimes they’re bringing in homeless people, people who are unconscious, women in labor, etc. I’m trying to think of something your local government politician would rather you weren’t allowed to do even more.
It might be better for them if they were purposely letting restaurants serve kittens and puppies at an all you can eat buffet.
I’ll put it this way, they’d probably rather everybody found out they were shagging the receptionist than find out that they purposely let the ER refuse service–and somebody’s Mom or baby died because of it.
Tar and feathers and torches and pitchforks all the way out of town.
Well, in the 90’s, a huge number of hospitals just closed their emergency rooms and redefined themselves as clinics/surgery centers/medical centers and solved that problem.
“Sorry, you have to go to County General for that”
Having taken my son ER myself – little kids with serious problems get to the doctor waaay before the “guy with a cold”.
From what I overheard the last time I was there, waits were hours and hours.
the hospitals would have devised a means of dealing with it. Not by dragging the dying out onto the sidewalk, but by improving their methodology for sorting and differentiating between actual emergencies, and “Mommy my tummy hurts” cases.
We are severely constrained by federal law in how we manage cases that “present to the Emergency Department”.
Like an old-fashioned nurse at a desk in the doorway with a list of questions.
Well, we have to give a “medical screening exam” to everyone who shows up. Its more involved than that, in most cases.
You go through that door, you go through this door.
If we were to tell someone to go to a clinic or any other kind of facility who had presented to our ED, we would violate federal law. Basically, we have to give an exam to every single person that walks through our ED door and we have to stabilize them, unless they need care we just don’t provide. We’re not allowed to transfer them or tell them to seek care elsewhere (unless they need care we just don’t provide). Once they show up and say “I sick”, they are our problem to solve, and there’s not much we can do about it.
Would hospitals benefit from having a built-in walk-in clinic solution for the non-ER types of treatment?
Most have the functional equivalent of a walk-in clinic more or less attached to their ER, but its still a hospital operation, which means its more expensive.
The best case scenario is this:
(1) Patient walks into ED with minor complaint.
(2) Patient is given a medical screening exam by a “licensed independent practitioner”, typically a doctor or advanced practice nurse. Triage (generally a few questions to get a handle on what’s going on) is not the same as a medical screening exam, which needs to be sufficient to diagnose the presenting problem. So you burn licensed provider time, diagnostics, etc.
(3) The exams shows, yup, a minor complaint. Theoretically, if it shows a non-emergent condition, you can kick the patient out of your hospital. Nobody does that (see, also, the tort of “patient abandonment”). The usual course is you go ahead and treat the patient, in the very costly way hospitals do. The other best-case option is to ask the patient if they wouldn’t prefer going to the walk-in clinic right outside the hospital (assuming you have one), and they say yeah, it will be faster and cheaper. Pro-tip: even when available, most patients don’t take the option.
It’s 9pm, the clinic is closed. I sick now.
So, my wife was on the Medicaid (maybe Medicare?) When she was going through Dialysis, etc.
Both programs serve a large number of people with serious illness. If my wife told me at 2 in the morning something was wrong, where do I take her?
Even if something happened during business hours, when I would call her primary, the nurse would say “take her to the ER, now”
Well, there is the rise of the Minute Clinics in pharmacies all over.
Thanks Ken for taking the time to write this article.
The tragedy of our current healthcare system is that we have linked health insurance with health care. Another tragedy is that we don’t view health care as a good or commodity to be provided but rather something that should be provided or at least heavily facilitated by the government.
This is why when someone like Ken or one one us us try to frame the debate in terms of allowing competition and getting rid of mandates people go apeshit and accuse us of wanting the poor to die in the streets. Once we get past and dismantale the idea that health care is a human right, we can actually have a productive discussion about health care reform.
When someone gives me the “healthcare is a right” formulation, I posit the following hypothetical :
There is a new medication.
It costs $1 Trillion.
Everyone who receives it will live 5 minutes longer than they would live if they did not receive it.
Does everyone have a “right” to receive it?
If they’re smart enough and intellectually honest, they accept that of course not, there’s inevitably a cost-benefit analysis… and so healthcare cannot be a “right” … and they support “death panels.” Usually they just say “that’s a ridiculous example” because they’re not intelligent to understand that it is ridiculous on purpose to illustrate the point.
You have to be a real simple minded fuck or a complete partisan hack to walk away from this coverage, especially the links provided, and not notice that much of the media are blatant mouthpieces for the Democrats.
They are utterly obsessed by the notion that Trump would “slander” their hero, his predecessor. They have gone nuts over it.
Trump saying something mean about their idol rises to the level of an impeachable offense.
Am I supposed to be mad?
It is not I am who am crazy…it is I who am MAD!!!!
we don’t view health care as a good or commodity to be provided but rather something that should be provided or at least heavily facilitated by the government.
You don’t die from putting off getting a new teevee for six months1!!!!!111!!11
But you will die of dehydration or starvation sooner than that!!!1!!elventy!!oneoneone!! YOU NOW MUST include food and water as a human right!!!!!!!!!!
in Chicago, people without the means will wander into a Cook County hospital and fill the ER.
It seems to me the hospital would have a huge incentive to keep those people from clogging up the ER, and divert them into an alternative treatment option. They evidently don’t. This indicates to me that some sort of an incentive exists which causes them to refrain.
Maybe it has to do with billing write-offs, maybe it has to do with something else. I don’t know, but it just bugs me.
A few additional thoughts, from the (limited) perspective of a hospital guy:
(1) Many hospitals can treat Medicare patients on pretty much a breakeven basis these days. For years, breaking even on Medicare was a financial goal for a lot of hospitals in trying to control their costs. At this point, I think most hospitals fall within a range of a few percentage points on either side of breaking even on Medicare.
(2) Medicaid is a huge loser for hospitals, with some things getting paid OK, and some getting paid at as low as 20% of the actual cost. That chart just looks wrong to me – I don’t know any hospitals that have a better margin/lower losses on Medicaid than on Medicare.
(3) Most commercial insurance pays at a percentage of Medicare rates. The chart makes it look like that percentage is 150 – 160%. In my experience which is limited, I know, that sounds way high. The hospitals I am familiar with would be delighted to get 125% of Medicare.
(4) The hidden cost of these programs is pretty big – friction in operations due to regulatory requirements, big billing and coding staffs, bullshit denials of payment, etc. Hospitals house large bureaucracies, a fair amount of which is driven entirely by Medicare and Medicaid.
(5) Most hospitals runs on pretty thin margins – 2 – 3%. A few do better, but not many. Insurance company “real” margins are impossible to get a handle on, but what they report tend to be pretty thin margins as well. Of course, a thin margin on a multi-billion dollar book is real money. Our rule of thumb is that insurance companies skim/hide a solid 15% of premium revenue on their books. Health systems generally are trying to get further upstream on revenue by going direct to employers or by having what amounts to their own insurance company, and when you cut the insurance companies out of the mix, there is more money and more margin to be had, assuming you are pricing and managing your risk well.
(6) Getting rid of the individual mandate is good, but the real problems inflicted by OCare on our health insurance industry come from (a) benefits mandates, (b) community rating, and (c) no medical underwriting. If you don’t get rid of those, you won’t solve the problem; they are the time tested recipe for a death spiral. The individual mandate was supposed to solve the death spiral problem, but it was always going to fail.
On “bullshit denial of payments”, I just got bitten on that. I had a procedure several years ago that was pre-cleared with the insurance company. After the fact they asked for some more information. After doing that dance for a while, they went away.
Then a couple of months ago they notified the hospital that they were not paying. So I got a bill for about $15k.
Now I have to deal with this crap. I’ll note again that the entire thing was pre-cleared with the insurance company exactly for the purpose of avoiding this sort of thing.
My opinion is that a big part of the problem with healthcare reform and most others is that it can’t come alone.
Assuming free market health care reform that reduce costs, these should come as a package with society wide free market reforms to increase economic growth and incomes so that people can actually afford the rates, even lower than that. And this just won’t happen, true free market reforms are politically untenable.
Also people need to understand the simple concept that you can’t save em all. That is just not possible. And if people think European socialized medicine systems save everyone who has a curable condition, they are deluded. Resources are not unlimited.
Resources are not unlimited.
When I’m talking to a smart person about this, I say “healthcare” is actually just as “healthcare good and services” and those goods and services have a cost of provision. Unless they are going to enslave the people providing those goods and services, there cannot be an unlimited “right” to “healthcare.”
I’ll note that in the countries that do attempt to enslave said workers, those workers just quit their healthcare jobs. Because, you know, they’re not actually slaves.
We are severely constrained by federal law in how we manage cases that “present to the Emergency Department”.
Thanks, RC. I’ll file that under “Regulation Constrains Innovation”.
To the point about costs not being distributed evenly geographically, I can personally attest to this.
I live in Florida, where the eastern half of the US sends their elderly to die. We have a huge medicare population. Seemingly every doctor has “not accepting new medicare patients” on their website. We also have a huge medicaid population – with lots of new immigrants (the legal kind) and an ordinary amount of poor folk, plus the medicaid expansion that pushes a lot of working families onto medicaid. I think three kids and 80k of income will put you on medicaid.
What does this mean for me? Well, those costs are so high that my private insurance plan costs went from about $650/mo before Obamacare to …. wait for it…. almost $2,000/mo this year. And that is with a $13,500 deductible. Let that number sink in for a moment. My deductible this year is more than my max out of pocket – including premiums – before Obamacare.
So thanks for that.
You just illustrated why it’s so important to keep Obamacare. Imagine those costs without its life saving succor.
Back when Obama(doesn’t)Care was just a bill, someone I know was telling me how wonderful it was going to be. I expressed strong skepticism that more bureaucracy and government spending would fix an industry that is already overloaded with those two things, but he insisted that it would finally fix healthcare and make it affordable for everyone.
Last year, I was making $11 per hour at a job that didn’t offer health insurance, and the cheapest plan I could find on the “marketplace” * was $135 per month. When I pointed out how this is really not helpful to me at all, the guy said, “eh, I’m in favor of spreading healthcare costs to everyone; we all end up paying for it anyway.”
Hmm… I thought this magical law was supposed to “make healthcare affordable”, not just spread the costs around (and actually increase them quite a bit). Maybe the “progressive” left should make it easier on themselves and just mount wheels on those goalposts.
* FYI: Healthcare.gov is still a malfunctioning piece of shit as of summer of last year.
Well, sounds like you’re a pup, no offense. That’s the idea behind Obamacare: young healthy people maybe shouldn’t be prioritizing their budget around healthcare, but if they don’t, the rich old people (and poor and really sick people) would have to pay more. That’s why there’s a mandate: otherwise young healthy people would (correctly) spend their scarce resources on things more becoming to that stage of life: dependable transportation and home ownership, for instance.
And that’s something I never see mentioned: opportunity cost. If young people are forced to subsidize everybody else, that means they don’t have that money to spend elsewhere, to wit housing, and if the premiums are so high, how can they afford babies?